Virtual cadavers can enhance anatomy education for students in the health sciences.
Introduction
Interpretation of computed tomography (CT) scans is a challenging skill to learn. Different organs of similar densities (e.g. the small bowel and the pancreas) can be indistinguishable on CT despite distinct appearances and functions in real life (O’Rourke et al., 2020). This can make it hard to understand normal and pathologic anatomy as well as hinder clinical decision making. Some studies have shown that problem-based sessions that employ CT scans can help students learn anatomy better (Bass et al., 2018; Rathan et al., 2022; Zumwalt et al., 2007). Additionally, in the wake of the COVID-19 pandemic, traditional methods of teaching anatomy, using in-person sessions, were abruptly stopped. Based on our group’s prior experience using radiation treatment planning software to teach anatomy for virtual medical students (Janopaul-Naylor et al., 2021), we developed a novel tool, which uses a virtual cadaver linked with CT images, to help teach the fundamentals of CT interpretation.
Informed by models of experiential learning (Gagné, 1965; Lawson, 1974), we developed a series of case vignettes to help students learn and retain fundamental skills in CT image interpretation of the upper abdomen. We targeted medical students without access to in-person anatomy labs due to the pandemic or who hadn’t yet completed their human anatomy course. Herein we report our preliminary findings from a hybrid in-person and virtual pilot group of medical students.
Methods
Virtual Cadaver Teaching Tool
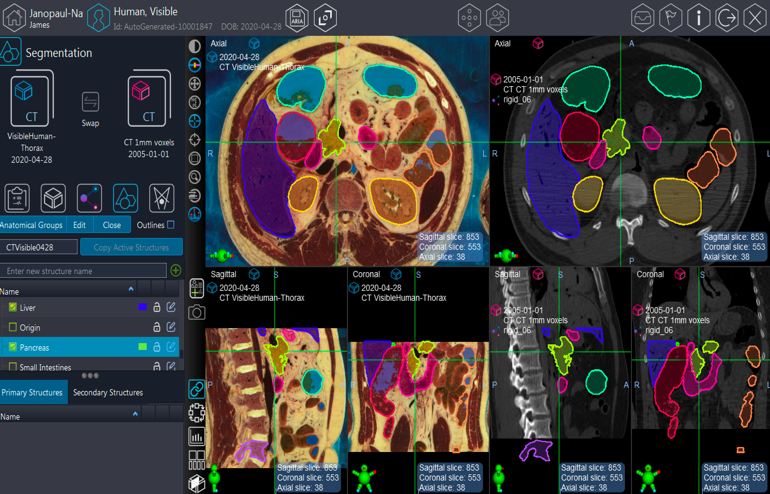
The images were retrieved from the Visible Human Project (The National Library of Medicine’s Visible Human Project, n.d.). This included 1,871 axial-oriented CT images with 1mm thickness as well as a corresponding series of 1,871 photographs of a cadaver with relatively normal anatomy that had been serially sectioned. These were uploaded into Velocity software, a radiation oncology treatment planning system (Velocity | Varian, n.d.). This allowed students and the facilitator to outline organs and areas of interest as well as to link the cadaver and CT images so that they could be viewed in parallel or overlayed on top of each other. Outlines of the major upper abdominal organs including liver, gallbladder, stomach, small and large bowel, pancreas, kidneys, spleen, bones, spinal cord, and vasculature are shown in a sample image in Figure 1.
Teaching Session Design
IRB review was waived as a program evaluation project. This was a pilot study with students invited from Emory School of Medicine’s Radiology Interest Group to participate in-person or virtually. The main learning objective was to identify abdominal organs and sub-structures on CT imaging. Students manually attempted to outline structures using different perspectives on the CT or virtual cadaver (e.g. axial, coronal, or sagittal views). Feedback was provided by facilitators throughout the single one-hour teaching session, with reference to the linked cadaver images. The cadaver images provided intuitive distinctions between organs such as the liver and the kidney whose borders on CT imaging can be unclear. We then discussed hypothetical cases of pathology involving different organs as well as how to think about improving the CT scan to facilitate clinical decision making. For example, oral contrast would help distinguish the small bowel from the pancreas or intravenous contrast could help identify blood vessels.
Program Evaluation
After the session, an anonymous survey was sent via email to participants. Questions assessed subjective confidence in upper abdominal anatomy as well as specific benefit of the teaching session and virtual cadaver in increasing confidence in anatomy. Additional questions gauged prior experience with anatomy and radiology, and year in medical school (Table 1).
Results and Discussion
Seven students (six male, one female) attended the pilot session (three virtually, four in person) with five of seven responding to the survey (71% response rate). The students were mostly in their 1st year of medical school (n=5) with one 2nd year medical student and one 3rd year medical student. All respondents reported moderate to high helpfulness of the session and increased confidence in identifying upper abdominal organs afterwards. One 1st year medical student found the cadaver images very helpful (20%), three students, including one 2nd year medical student and two 1st year medical students, found them moderately helpful (60%), and one 3rd year medical student found them not helpful (20%), indicating that the session may be most beneficial for earlier trainees.
Qualitatively, students were highly engaged throughout the session. Two students, including one who had started clinical rotations, mentioned how the discussion helped them think about imaging orders and how to optimize imaging decisions for different patient scenarios. Four students stayed to ask additional questions after the initial allotted one-hour session. Two students reached out after the session about instructions on how to access the tool going forward.
Of note, most students (n=4) were interested in radiology as a potential residency or had spent time shadowing in a radiology department either before or during medical school.
Prior work has shown the value of medical imaging training for physicians in multiple specialties (Marsland et al., 2018). One key benefit of the Velocity software used in this session is the ability for students to draw and manually identify organs independently. On one-hand, the autonomy presents a challenge, particularly initially as students may not know how to use the software or have intuition about where organs were located. However, on the other hand, the ability to control the imaging increased engagement. Furthermore, students gained confidence by comparing their own outlines to the facilitator’s or were able to rapidly identify errors and discuss ways to avoid mis-identifying that organ in the future. In contrast, traditional slide-based didactics only allow a limited number of images, pre-selected by the facilitator, and limit the autonomy of students to explore the anatomy and structures at their own pace. We think that encouraging learners to manipulate 3-dimensional imaging (e.g. CT or MRI scans) as part of teaching sessions better mimics real-world practice and could increase participation, engagement, and retention.
Some of the limitations of this project include the number of cadaver images available, technical challenges with setup, and sample size. The Visible Human Project has open-source male and female datasets that include cadaver and CT imaging of the pelvis, abdomen, and thorax. However, there are not robust cadaver image sets of different pathologies. A major hurdle for implementation of this project was formatting the CT and cadaver images so that the Velocity software could interpret them. Finally, we had a small and potentially biased pilot group, and so it is unclear if the favorable impressions are generalizable to students not interested in radiology or learners at different levels of training.
Future directions include identifying groups that could benefit from additional resources for imaging and anatomy teaching. For example, cadaver images, with better visualization of blood vessels, may help surgical residents prepare for complex operations. Alternatively, medical students transitioning to emergency medicine residency could use this tool to help with rapid interpretation of CT images. In general, this could be a helpful introduction or refresher for a variety of health professionals that rely on CT imaging for their clinical practice. For schools without an anatomy lab, the use of cross-sectional imaging of a human cadaver could provide an alternative teaching resource. There is also a need for additional evaluation of the training with a larger sample size and greater depth of quantitative and qualitative evaluation measures.
Conclusions
We demonstrated that a small pilot study of hybrid in-person and virtual medical students could use human cadaver imaging to facilitate learning the basics of CT images of the upper abdomen. Future sessions may better elucidate benefits, limitations, and additional applications of this novel tool.
Acknowledgments
The authors received no grant support for this work. The authors declare that we have received no payment or services from any third party to support this work.
Figure 1. Radiation treatment planning interface showing cross-sectional images of linked human cadaver and CT images. Outlined organs include Colon, Duodenum, Kidneys, Liver, Lumbar Spinal Vertebrae, and Pancreas. Learners are able to scroll through any of the orthogonal planes as well as personally outline organs through this software.
| Table 1: Anonymous survey sent to participants | |||||
| Question | Response Type | Response Options | |||
| After this session, how confident are you in identifying upper abdominal structures? | Multiple Choice | Not at all confident | Moderately Confident | Very Confident | |
| How helpful was the teaching session at increasing your confidence in upper abdominal anatomy? | Multiple Choice | Not at all confident | Moderately Confident | Very Confident | |
| How helpful was the virtual cadaver in clarifying structures on the CT scan? | Multiple Choice | Not at all confident | Moderately Confident | Very Confident | |
| How much did you learn from this course | Multiple Choice | Almost nothing | A little bit | Quite a bit | A tremendous amount |
| What year in medical school are you | Multiple Choice | 1st Year | 2nd Year | Other | |
| What background do you have with radiology | Free Response | ||||
| Please provide any feedback (positive, neutral, or negative) about this session | Free Response |
Bass, R. Z., Morgan, D. E., & Brooks, W. S. (2018). A Case of Pancreatic Cancer: Abdominal Anatomy Team-Based Learning Module for Medical Students. MedEdPORTAL : The Journal of Teaching and Learning Resources, 14, 10700. https://doi.org/10.15766/MEP_2374-8265.10700
Gagné, R. M. (1965). The Learning of Concepts. The School Review, 73(3), 187–196. https://doi.org/10.1086/442739
Gagne, R. M., Briggs, L. J., & Wager, W. W. (1992). Principles of instructional design (4th ed.). Harcourt Brace Jovanovich College Publishers.
Janopaul-Naylor, J., Qian, D., Khan, M., Brown, S., Lin, J., Syed, Y., Schlafstein, A., Ali, N., Shelton, J., Bradley, J., & Patel, P. (2021). Virtual Away Rotations Increase Access to Radiation Oncology. Practical Radiation Oncology, 11(5), 325–327. https://doi.org/10.1016/j.prro.2021.06.002
Lawson, T. E. (1974). Gagne’s learning theory applied to technical instruction. Training & Development Journal, 28, 32–40.
Marsland, M. J., Tomic, D., Brian, P. L., & Lazarus, M. D. (2018). Abdominal Anatomy Tutorial Using a Medical Imaging Platform. MedEdPORTAL : The Journal of Teaching and Learning Resources, 14, 10748. https://doi.org/10.15766/MEP_2374-8265.10748
O’Rourke, J. C., Smyth, L., Webb, A. L., & Valter, K. (2020). How Can We Show You, If You Can’t See It? Trialing the Use of an Interactive Three-Dimensional Micro-CT Model in Medical Education. Anatomical Sciences Education, 13(2), 206–217. https://doi.org/10.1002/ASE.1890
Rathan, R., Hamdy, H., Kassab, S. E., Salama, M. N. F., Sreejith, A., & Gopakumar, A. (2022). Implications of introducing case based radiological images in anatomy on teaching, learning and assessment of medical students: a mixed-methods study. BMC Medical Education, 22(1). https://doi.org/10.1186/S12909-022-03784-Y
The National Library of Medicine’s Visible Human Project. (n.d.). Retrieved December 11, 2022, from https://www.nlm.nih.gov/research/visible/visible_human.html
Velocity | Varian. (n.d.). Retrieved December 12, 2022, from https://www.varian.com/products/interventional-solutions/velocity
Zumwalt, A. C., Marks, L., & Halperin, E. C. (2007). Integrating gross anatomy into a clinical oncology curriculum: the oncoanatomy course at Duke University School of Medicine. Academic Medicine : Journal of the Association of American Medical Colleges, 82(5), 469–474. https://doi.org/10.1097/ACM.0B013E31803EA96A
James Janopaul-Naylor MD
Resident, Emory University School of Medicine, jjanopa@emory.edu
Naba Ali MD
Resident, Emory University School of Medicine
Jolinta Lin MD
Associate Professor in the Department of Radiation Oncology, Emory University School of Medicine
EDUARD SCHREIBMANN PHD
Associate Professor in the Department of Radiation Oncology, Emory University School of Medicine
PRETESH PATEL MD
Associate Professor in the Department of Radiation Oncology, Emory University School of Medicine