Research productivity during intense health sciences training is influenced by each individual’s past research experience as well as future career plans. Trainees may face common barriers such as restricted time and inadequate infrastructure, which reduce opportunities to engage in research activities and explore different areas of interest. Individuals who manage health sciences trainee programs should consider opportunities to reduce research barriers.
Abstract
Introduction: Research is essential for the professional development of otolaryngology residents. Research productivity has been positively correlated with increased academic employment opportunities and improvement in clinical practice. However, trainees at this stage of their career face significant obstacles due to intense working hours and lack of support and guidance.
Methods: Research productivity at different stages of training was assessed for otolaryngology residents and alumni at a single institution using Scopus as search tool. Publication count, h-index score, and citation count were evaluated for each individual and subsequently analyzed in relation to research background (i.e. existence or absence of pre-residency dedicated research experience [DRE]) among residents and fellowship and practice setting among alumni. Surveys inquiring on research barriers evaluated the perspective of the institution’s resident group and faculty.
Results: For residents, pre-residency DRE proved to be associated with a greater median of total publication count [DRE: 9.00 (8.00-13.50) vs No DRE: 4.00 (2.00-6.00)] (p=<0.001) and research productivity throughout residency [DRE: 3.00 (2.50-8.00) vs No DRE: 1.00 (1.003.00)] (p=0.022). When compared to general and private practice otolaryngologists, fellowship trained alumni and those in academic practice evidenced greater total publication count with a median of 10.0 (7.00-18.00) (p=<0.001) and 16.00 (8.50-20.50) (p=0.004), respectively. Through the survey, time was designated as the primary barrier for research productivity.
Conclusion: Research productivity often faces obstacles such as constraints in time and infrastructure. It is crucial to acknowledge that trainees have diverse research backgrounds and interest in pursuing an academic practice, which can influence their participation in research.
Introduction
Research plays a significant role in the academic growth of resident physicians and engagement in scholarly activities has shown to improve clinical performance (Bechtold et al., 2017; Noble et al., 2018). Research experience is highly valued on the job market, including for clinical fellowships and academic positions (van Schalkwyk et al., 2017). Additionally, prolonged dedicated research time during a surgical residency stands as a predictor of academic success and grant acquisition (Benesch et al., 2022). Yet residents may lack sufficient exposure to research along their training as they face specific obstacles that prevent the development of their project ideas.
Research productivity of resident physicians can be influenced by multiple barriers, including lack of time, infrastructure, interest, mentorship, and/or funding. Surgical residency represents an increase in clinical responsibilities and working hours. In 2019, the Accreditation Council for Graduate Medical Education (ACGME) reported an increase in work hours of otolaryngology residents, averaging more than 80 hours a week (Shah et al., 2023). Moreover, an appropriate infrastructure represented by equipment, facilities, resources, and services (e.g. biostatistics consultation) might not be readily available for trainees, limiting their ability to get involved and conduct advanced research (Tsikis et al., 2019). Research barriers such as lack of personal interest and mentorship have also been previously studied, as curiosity and experience are fundamental in the development and completion of projects (Fournier et al., 2019). Lastly, a lack of funding through institutional or departmental support serves as disincentive for project execution and conference participation.
Given the importance of research as part of clinical and academic evolution during medical training, this study seeks to assess how research background, fellowship training, and postresidency practice shape research productivity along different stages of training. Moreover, the study evaluates and reflects on different research barriers faced by physicians during residency.
Materials and Methods
Research Productivity Review
After obtaining approval form the Institution Review Board (No. STUDY00005605), a retrospective review was conducted on the research output from the institution’s current resident group (n=20) and alumni between July 2013 and July 2022 (n=35). Total publication count, preresidency publication count, residency publication count, h-index, and number of citations were collected for each individual using Scopus database, accessed in March 2024. Pre-residency publication count publications produced during undergraduate, master or doctorate programs, or medical school, before otolaryngology residency training. Information on the research background of the current resident group was also gathered.
Research background is defined by the existence or absence of dedicated research experience (DRE) before the initiation of medical residency. During the DRE, individuals had protected time protected time for research as part of a research rotation or research fellowship. In addition, post-residency publication count, type of fellowship, and practice setting were collected for alumni. Post-residency publication count included publications produced after completion of the five year-long otolaryngology residency.
Distribution of Surveys
A survey was presented to 14 otolaryngology residents, including first to fifth year residents within the sample. This survey covered topics related to their value of research, the department’s support of research, career plan, and barriers for research development. Additionally, a survey was conducted among 23 Otolaryngology faculty members to assess their perspective on both their personal and the resident’s barriers for research.
Data Analysis
Survey analysis was described through count (percentages) and quotations from open ended survey questions. Quantitative data was presented using median (inter-quantile range [IQR]). Normal distribution was assessed through a Shapiro-Wilk test. Assuming the data was non-normally distributed, Kruskal-Wallis and Mann-Whitney U tests were employed for analysis of quantitative variables. A Spearman correlation analysis was used to evaluate the association between pre-residency research productivity and number of publications during residency. This same method was applied for the analysis of research output based on each resident’s training stage (intern [PGY1], n=4; junior [PGY 2 and 3], n=8; and senior years [PGY 4 and 5], n=8). Data was analyzed and graphed using SPSS Version 28.0 (SPSS Software, Chicago, IL, USA). A p-value inferior to 0.05 was deemed significant for all statistical tests.
Results
Research Output of the Resident Group
The current otolaryngology resident group is composed of 20 trainees, with a distribution of 4 (20.00%) individuals per residency year. Of these, 7 (35.00%) trainees had DRE prior to entering residency. The median of total and pre-residency publication count per trainee were 6.50 (2.50-8.50) and 3.00 (1.00-6.00), respectively (Table 1). A Spearman correlation analysis evaluated the cumulative number of published manuscripts during residency based on each resident’s training stage: intern, junior, and senior. A positive correlation was established; however, this correlation did not reach significant proportions (ρ=0.315; p=0.088).

Trainees with DRE prior to entering residency had a significantly higher overall publication count with a median of 9.00 (8.00-13.50) publications compared to 4.00 (2.00-6.00) in those without pre-residency DRE (p=<0.001). This trend was also observed across other variables, including pre-residency publication count, first-authorship, and h-index score (Table 2).
Pre-residency DRE also proved to have a positive impact on research productivity throughout residency as trainees with research experience had a median of publication count during residency of 3.00 (2.50-8.00), compared to 1.00 (1.00-3.00) for those without a research background (p=0.022). (Table 2).
Research Output of Alumni
Between July 2013 and July 2022, the institution had 35 otolaryngology graduates. Of these, 19 (54.29%) alumni entered private practice and 16 (45.71%) delved into academic careers. After residency, fellowship training was pursued by 25 (71.43%) alumni whereas 10 (28.57%) opted for general otolaryngology. Fellowships in head and neck surgery and facial plastics and reconstructive surgery were the most commonly pursued, with a total of 7 (20.00%) and 6 (17.14%) alumni, respectively.

Engaging in fellowship training was associated with a significant increase in the total publication count, with a median of 10.00 (7.00-18.00) publications in fellowship trained graduates compared to 3.50 (1.00-7.00) in general otolaryngologists (p=<0.001) (Table 3).

A significant difference was also observed. in post-residency publication count (p=<0.001), h-index score (p=0.008) and number of citations (p=0.007) (Table 4).
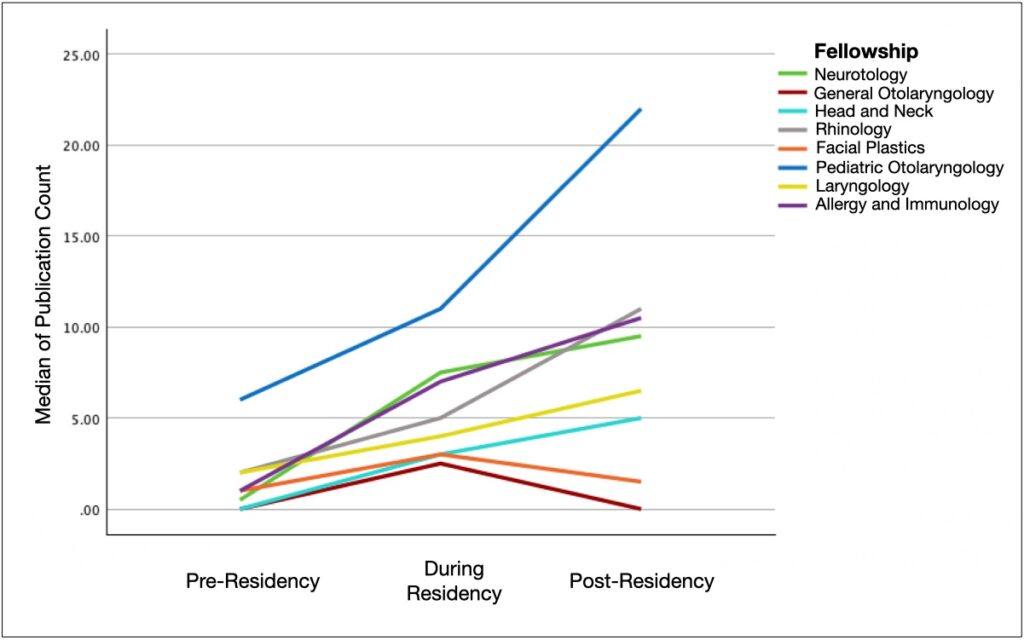
When the types of fellowships were compared, a significant difference was observed in total publication count (p=0.043), but not in residency publication count (p=0.068), h-index score (p=0.062), and citation number (p=0.062) (Table 4). Alumni research productivity by fellowship and training stage (pre-residency, during residency, and post-residency) is illustrated in Figure 1A. A Spearman correlation analysis revealed a significant positive correlation between the number of publications prior to residency and the publication count during residency across all graduates, independent of fellowship training or type of practice (ρ=0.438; p=0.008).

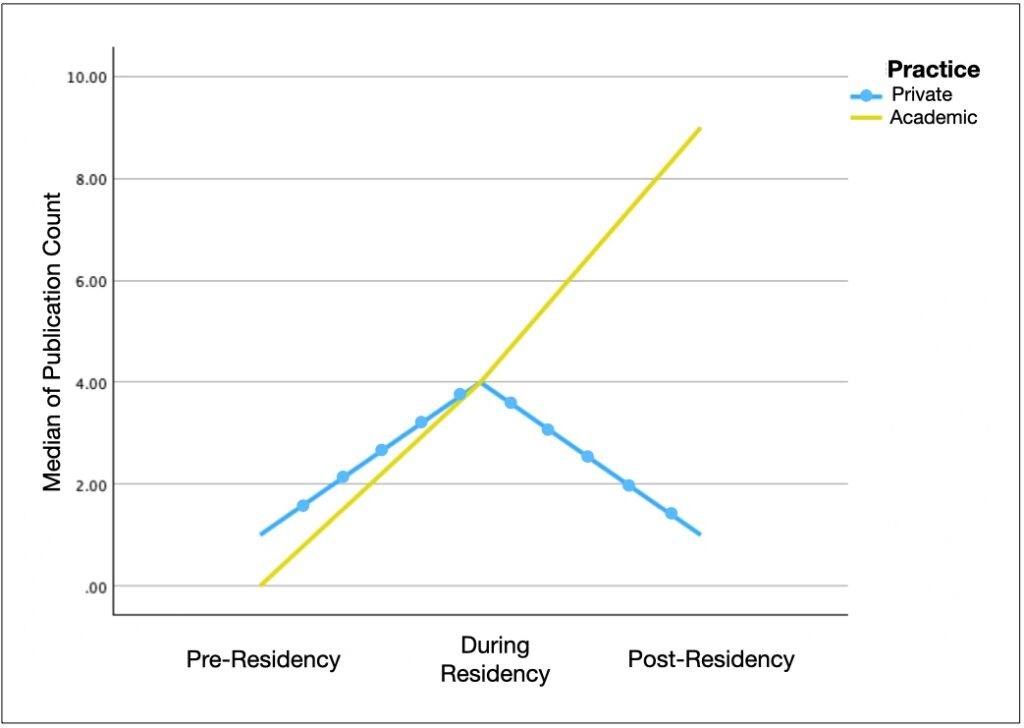
Among graduates, the type of practice proved to influence the overall research productivity and post-residency publication count. Surgeons that developed a career in private practice had a median total publication count of 7.00 (3.00-8.00) whereas those with an academic practice had median of 16.00 (8.50-20.50) (p=0.004) (Table 5). Nonetheless, citation number, h-index score, and residency publication count did not differ significantly between the two groups.

Figure 1B illustrates research productivity across each stage of training based on practice setting.
Resident Survey
Fourteen otolaryngology residents at different stages of their training were assessed through a multiple-choice survey. Among them, 2 residents (14.29%) considered private practice as their career plan, 5 (35.71%) aimed for an academic path, and 7 (50.00%) were still undecided. Two trainees (14.29%) ranked research as a low priority in their educational path, 9 (64.29%) considered it of moderate importance, and 3 (21.43%) placed a high value on it. From the resident perspective, 4 individuals (28.57%) reported that the department promoted a research culture above the average, 2 (14.29%) viewed this support as average, 7 (50.00%) considered it below average, and 1 (7.14%) indicated that the support was insufficient.
Barriers for Resident Research
When questioned about which barriers were more consistently an obstacle for their research performance, the entire cohort 14 (100.00%) unanimously agreed that time was the primary factor haltering their productivity. Infrastructure was positioned as the second most prominent barrier by 7 trainees (50.00%). Furthermore, funding, mentorship, and interest were each mentioned as barriers by 2 members (14.29%) of the group (Table 6). Moreover, two trainees provided an insight into the resident perspective relative to research and their personal priorities by mentioning, “I like research but find I am not prioritizing it as much because I have so little time to devote to things I prioritize more (family, friends)” and “Research to me is a necessary part of career advancement, but I value clinical growth/duties far more”. These perspectives were consistent across the resident group who participated in the survey.
Faculty Survey
Twenty-three otolaryngology faculty members were evaluated both on their personal involvement in research and their perception of barriers in resident research. Among the faculty members included in the survey, 8 (34.78%) stated that research had a minimal role in their practice, 9 (39.13%) considered it to have a moderate role, and 6 (26.09%) described it to be extensive. The most common barriers to their own research development included time and infrastructure, as pointed out by 12 (52.17%) and 10 (43.48%), respectively. Fifteen members (65.22%) believed that the department encouraged research, whereas 8 (34.78%) perceived the support as insufficient.
Barriers for Resident Research
Faculty members were surveyed on their perception of the program’s resident research productivity. Thirteen individuals (59.09%) established resident productivity as minimal whereas 9 (40.91%) perceived it as moderate. In the faculty survey, time was also established as the most common obstacle that residents face when working on research projects. However, differing from the residents’ perspectives, faculty members identified a lack of interest as the second most significant factor impeding resident productivity (Table 6).

DISCUSSION
Research has an important role in the academic growth of residents and scholarly requirements are now a firm component of accredited residency programs. The ACGME stated that residents should provide a manuscript for publication in a peer-reviewed journal by the end of their training. Research productivity has shown a positive association with clinical performance and rate of employment, particularly in terms of fellowship and academic positions (Haas et al., 2023). As is noted across the United States, residency is a highly demanding training stage, and trainees may encounter various obstacles as they attempt to initiate and evolve a research project. Thus, identifying the barriers residents face has become critical.
While evaluating the current otolaryngology resident team, a significant association between DRE prior to residency and research productivity during residency was established. This was indirectly supported by the positive correlation between the alumni’s pre-residency publication count and productivity throughout residency. Also, h-index score and first authorship were significantly higher in trainees with prior DRE, both of which are highly valued in the academic setting (Ashfaq et al., 2018). In the literature, similar results were presented for the ophthalmology field by Pur et al., (2024) as they found greater research productivity during residency among those who had at least one publication pre-residency. Furthermore, they were able to establish an association between pre-residency research productivity and immersion in fellowship training and academic careers (Pur et al., 2024). These findings highlight the importance of identifying which trainees require additional support and mentorship, providing them with valuable assets necessary for an academic path.
Overall research productivity was greater in two scenarios: fellowship trained physicians and academic-bounded practitioners. Alumni who pursued a fellowship after residency evidenced a higher publication count and h-index score. In addition, when evaluating research productivity among fellowship types, a significant difference was established across total publication count. This difference was primarily influenced by the incredible publication output of pediatric otolaryngologists. Interestingly, this correlates with findings by Kirubalingam et al., who demonstrated a significant increase in the number of articles published in pediatric otolaryngology from 2013 to 2021 (Kirubalingam et al., 2023). As previously mentioned, practice also influenced total publication count, and this is explained by the increased funding and infrastructure academic otolaryngologists have access to.
This study revealed that both time and infrastructure support are seen as the main elements affecting research productivity. Residents expressed favoring a balance between clinical work and personal life, which aligns with findings in the published literature (Merino et al., 2023). Methodological support is also a relevant barrier, primarily among residents who have had less experience with research. Furthermore, faculty members pointed out that a lack of focused interest also curtailed the research process, emphasizing the need for direct mentorship and guidance starting from early stages of training. Ahn et al. studied the interest in research among orthopedic surgery residents and found an inclination towards clinical investigation given its direct relevance to their practice (2010). In addition, they found interest was positively correlated with previous research experience, first authorship, and age (Ahn et al., 2010).
Time as a Barrier
During surgical residency, time is constrained by work-hour restrictions, surgical caseload, clinical responsibilities, educational requirements, and social needs (Merino et al., 2023). The perception of time as the primary barrier for research is a consistent finding across other medical specialties, including ophthalmology and plastic surgery (Al-Taha et al., 2017; Pur et al., 2024). As shared by the group of residents included in this study’s survey, although there is a genuine motivation for conducting research, surgical and clinical evolution is prioritized, and their limited time off duty favors quality time with family and friends. Allocating a specific time frame for research is commonly proposed by residency programs, however there is no consensus on how long this protected time should be and how it should be distributed. Programs may advocate for month-long dedicated time, while some others have implemented weekly dedicated time (Clark et al., 2021). Moreover, to encourage a career path leading to academic positions and the development of clinician-scientists, certain programs have chosen to add an entire year dedicated to research (Stevenson et al., 2017). This year can be structured as a standalone program or aimed at completing a master’s or PhD degree (Zuo et al., 2020). In general, published studies agree strictly established protected research slots embedded in the residency educational curriculum should be implemented to help trainees integrate research into their practice (Al Absi et al., 2024; Al-Taha et al., 2017).
Infrastructure as a Barrier
Residents oftentimes find themselves facing restrictions related to study logistics. For example, statistical analysis may require personal skills or a specialized statistician. Either of these are provided by a robust research infrastructure. Moreover, equipment, facilities, and services required for the continuation of projects should be readily available during protected research rotations given the limited time trainees have away from clinical work. Teamwork among residents is also an important component of the research infrastructure. Cultivating a culture of research within the department is particularly important when encouraging faculty and residents to engage in mutual scholarly activities (Nocera et al., 2016). This means equipping them with the necessary tools to facilitate research workflow. Studies have shown a benefit in research productivity with infrastructure improvement strategies such as including dedicated research staff in the department, providing access to experienced statisticians, and creating multidisciplinary research teams (Seehusen et al., 2023).
Mentorship as a Barrier
Creating a mentor-mentee relationship can have a positive impact in both clinical and scholar growth, and its success relies on mutual interests and compatible working style (van Schalkwyk et al., 2017). In addition, each mentee might have different needs given their academic background, and these should be acknowledged by those providing guidance. Aside from nurturing a resident’s curiosity, mentors may also serve as point of contact for other specialists that can further collaborate with their expertise. Mentorship should be established as early as possible, meaning intern year or second year of residency, to take advantage of such guidance in the process of developing a research question. From there on, a sense of commitment is developed, and the execution of the project can be supervised along the way. Furthermore, peer-to-peer mentorship should also be considered as senior residents themselves can serve as mentors and collaborate in projects with interns and junior residents (Chiu et al., 2019). Of note, the results revealed a nearly significant direct trend in the correlation between residency training stage and the cumulative publication count during residency, emphasizing on the experience that can be passed on from senior residents to juniors and interns.
Interest as a Barrier
For residents, having a clear interest can help develop a research question that fulfills their intellectual curiosity. Typically, those interested in pursuing an academic path have greater motivation. As was noted in this study’s results, residents in the first years of residency have not yet decided which career path matches their expectations. Mentorship may be the most straightforward strategy to increase interest as mentors contribute with a broader and more indepth perspective of a particular field.
Although the majority of residents in this study value research as an important aspect for their training, a lack of interest evolves secondary to time and infrastructure limitations. Incentives such as financial support and awards have both been proposed as means to increase interest in research work. Haas et al. mentioned awards were associated with higher rate of project publication (2023).
Funding as a Barrier
Funding resident research is paramount for the execution of projects and participation in scientific meetings. The lack of financial support can work as a disincentive for research and should be adequately addressed. Funding research represents a significant expense, especially for those who are not supported by external entities such as the National Institutes of Health (NIH). Skube et al. proposed a strategy in which residents receive partial support through partnership with the local industry (Skube et al., 2018). They were successful in this approach by facilitating a paid immersion course in which the industry could have a first-hand experience in the operating room and clinical environment completely guided by residents. Finally, competing for grant funding can be challenging and requires a significant effort. Seehusen et al. showed making grant writing expertise available to trainees and faculty members increased the level of research capacity in up to 75% of the assessed family medicine departments (2023). For this study, research capacity was evaluated based on the number of peer-reviewed publications, research grants, percentage of departmental funding allocated to research, among other variables (Seehusen et al., 2023).
Limitations
This study primarily represents a self-assessment of a single institution’s otolaryngology residency program. Although valuable insights can be extracted from the analysis, further investigation is needed on a larger sample, considering each program is diverse in their approach to research requirements. The same methodology could be applied to programs with a research track, establishing how longer dedicated research periods influence productivity and career evolution.
CONCLUSION
Research productivity during residency can be challenging, essentially as a result of time and infrastructure limitations. Additionally, it is important to consider that each trainee comes from a different research experience, and this can influence their interest and publication output during residency.
ACKNOWLEDGMENTS
The authors received no grant support for this work and declare they have no conflicts of interest in regard to this work.
Ahn, J., Donegan, D. J., Lawrence, J. T., Halpern, S. D., & Mehta, S. (2010). The future of the orthopaedic clinician-scientist: part II: Identification of factors that may influence orthopaedic residents’ intent to perform research. J Bone Joint Surg Am, 92(4), 10411046. https://doi.org/10.2106/jbjs.I.00504
Al Absi, D. T., Yousuf, K., Aljaberi, K., AlBreiki, R., Simsekler, M. C. E., Omar, M. A., Ayathan, S., Mehmood, T., Anwar, S., & Kashiwagi, D. T. (2024). Barriers Preventing Medical Trainees from Active Participation in Research Activities. J Multidiscip Healthc, 17, 1513-1522. https://doi.org/10.2147/jmdh.S447948
Al-Taha, M., Al Youha, S., Al-halabi, B., Stone, J., Retrouvey, H., Samargandi, O., Efanov, J. I., Stein, M., Morzycki, A., Augustine, H., Bougie, E., Song, D., Power, H., Diaz-Abele, J., Symonette, C., Noland, M., Coroneos, C., Voineskos, S., Vorstenbosch, J., . . . Williams, J.
- (2017). Barriers and Attitudes to Research Among Residents in Plastic and Reconstructive Surgery: A National Multicenter Cross-Sectional Study. Journal of Surgical Education, 74(6), 1094-1104. https://doi.org/https://doi.org/10.1016/j.jsurg.2017.04.004
Ashfaq, A., Kalagara, R., & Wasif, N. (2018). H-index and academic rank in general surgery and surgical specialties in the United States. J Surg Res, 229, 108-113. https://doi.org/10.1016/j.jss.2018.03.059
Bechtold, J. E., Williams, B. R., Weinstein, S. L., Polly, D. W., Pugely, A. J., Buckwalter, J. A., Albanese, S. A., Bozic, K. J., & Snyder, B. D. (2017). The Pursuit of Scholarship: Why We Should Care About Resident Research. J Bone Joint Surg Am, 99(22), e119. https://doi.org/10.2106/jbjs.16.01502
Benesch, M. G. K., Mathieson, A., & Pace, D. E. (2022). Research and surgical residency: moving beyond one-and-done projects and motivating for scholarly excellence. Can J Surg, 65(4), E485-e486. https://doi.org/10.1503/cjs.013821
Chiu, A. S., Pei, K. Y., & Jean, R. A. (2019). Mentoring Sideways-A Model of Resident-to-Resident Research Mentorship. J Surg Educ, 76(1), 1-3. https://doi.org/10.1016/j.jsurg.2018.05.016
Clark, S. C., Sanborn, L., Brown, S. M., Trojan, J. D., & Mulcahey, M. K. (2021). Research Productivity of Orthopaedic Sports Medicine Fellowship Programs in the United States. Arthrosc Sports Med Rehabil, 3(4), e997-e1002. https://doi.org/10.1016/j.asmr.2021.02.007
Fournier, I., Stephenson, K., Fakhry, N., Jia, H., Sampathkumar, R., Lechien, J. R., Melkane, A. E., Bahgat, A. Y., De Carvalho Lopes, K., Kennel, T., Teissier, N., & Ayad, T. (2019). Barriers to research among residents in Otolaryngology – Head & Neck Surgery around the world. European Annals of Otorhinolaryngology, Head and Neck Diseases, 136(3, Supplement), S3-S7. https://doi.org/https://doi.org/10.1016/j.anorl.2018.06.006
Haas, D. M., Hadaie, B., Ramirez, M., Shanks, A. L., & Scott, N. P. (2023). Resident Research Mentoring Teams: A Support Program to Increase Resident Research Productivity. J Grad Med Educ, 15(3), 365-372. https://doi.org/10.4300/jgme-d-22-00499.1
Kirubalingam, K., Dzioba, A., Chan, Y., & Graham, M. E. (2023). Trends in otolaryngology publications: a 9-year bibliometric analysis of articles published in Journal of Otolaryngology-Head and Neck Surgery. J Otolaryngol Head Neck Surg, 52(1), 17. https://doi.org/10.1186/s40463-022-00619-0
Merino, T., Rojas, V., Fuentes-López, E., Sánchez, C., Pizarro, M., Fuentes-Cimma, J., Cifuentes, L., Cuello, M., Carvajal, J., Balcells, M. E., & Riquelme, A. (2023). Barriers for research activities in residency programs: A mix-methods study. Medwave, 23(1), e2627. https://doi.org/10.5867/medwave.2023.01.2627
Noble, C., Billett, S. R., Phang, D. T. Y., Sharma, S., Hashem, F., & Rogers, G. D. (2018). Supporting Resident Research Learning in the Workplace: A Rapid Realist Review. Acad Med, 93(11), 1732-1740. https://doi.org/10.1097/acm.0000000000002416
Nocera, R., Ramoska, E. A., & Hamilton, R. J. (2016). Building a resident research program in emergency medicine. Intern Emerg Med, 11(2), 245-248. https://doi.org/10.1007/s11739-015-1354-x
Pur, D. R., Kryshtalskyj, M. T., Hutnik, C. M. L., & Bursztyn, L. (2024). Association of preresidency publications with research productivity in residency, fellowship, and academic career choice among Canadian ophthalmologists. Can J Ophthalmol. https://doi.org/10.1016/j.jcjo.2024.02.004
Seehusen, D. A., Koopman, R. J., Weidner, A., Kulshreshtha, A., & Ledford, C. J. W. (2023). Infrastructure Features Associated With Increased Department Research Capacity. Fam Med, 55(6), 367-374. https://doi.org/10.22454/FamMed.2023.736543
Shah, H. P., Salehi, P. P., Ihnat, J., Kim, D. D., Salehi, P., Judson, B. L., Azizzadeh, B., & Lee, Y. H. (2023). Resident Burnout and Well-being in Otolaryngology and Other Surgical Specialties: Strategies for Change. Otolaryngol Head Neck Surg, 168(2), 165-179. https://doi.org/10.1177/01945998221076482
Skube, S. J., Arsoniadis, E. G., Jahansouz, C., Novitsky, S., & Chipman, J. G. (2018). Supplementing Resident Research Funding Through a Partnership With Local Industry. J Surg Educ, 75(4), 907-910. https://doi.org/10.1016/j.jsurg.2018.01.006
Stevenson, M. D., Smigielski, E. M., Naifeh, M. M., Abramson, E. L., Todd, C., & Li, S. T. (2017). Increasing Scholarly Activity Productivity During Residency: A Systematic Review. Acad Med, 92(2), 250-266. https://doi.org/10.1097/acm.0000000000001169
Tsikis, S., Fleishman, A., Chaikof, E. L., & Rodrigue, J. R. (2019). Design and Implementation of an Infrastructure Program to Support Clinical Research in Surgery. Journal of Surgical Research, 241, 264-270. https://doi.org/https://doi.org/10.1016/j.jss.2019.03.044
van Schalkwyk, G. I., Katz, R. B., Resignato, J., van Schalkwyk, S. C., & Rohrbaugh, R. M. (2017). Effective Research Mentorship for Residents: Meeting the Needs of Early Career Physicians. Acad Psychiatry, 41(3), 326-332. https://doi.org/10.1007/s40596-016-0625-9
Zuo, K. J., Meng, Y., Gordon, L., Saun, T. J., Mazine, A., Ahuja, C. S., Lipsman, N., Rutka, J. T., & Fehlings, M. G. (2020). Navigating the Postgraduate Research Fellowship: A Roadmap for Surgical Residents. J Surg Res, 256, 282-289. https://doi.org/10.1016/j.jss.2020.06.054
Alejandra Rodas, MD
Post-Doctoral Research Fellow, Department of Otolaryngology
Head and Neck Surgery, Emory University School of Medicine, Atlanta, GA
ORCID: 0000-0002-7868-7098
Anita B. Sethna, MD
Associate Professor, Program Director, Chief of Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology
Head and Neck Surgery, Emory University School of Medicine, Atlanta, GA
ORCID: 0009-0008-9840-4615
Published: 1/14/25