In this “How-to,” we describe the foundational development of the Medical Education Transformation process aimed at empowering ESOM (Emory School of Medicine) learners to be change agents capable of addressing evolving health challenges by reimagining curricula and co-curricular elements across all ESOM learners and all ESOM degree programs.
INTRODUCTION
Emory School of Medicine (ESOM) educational programs are known for producing outstanding clinical providers and scientists. When the MD program curriculum was last revised in 2007, Emory was among the first in the country to shorten the pre-clinical period, introduce early clinical exposure, implement a research block, develop a comprehensive service-learning curriculum, and prioritize our students’ health and wellness. During the 2021 Emory School of Medicine (ESOM) strategic planning process, a group of 120 education thought leaders developed a vision and goals that would advance our educational programs even further. With this transformation, we are again taking the lead. We believe we are one of the first medical schools in the country to reimagine and transform the curricula for all six of our degree programs – Bachelor of Medical Science Medical Imaging (BMSc), Doctor of Medicine (MD), Doctor of Physical Therapy (DPT), Master of Medical Science (MMSc), Master of Medical Science Genetic Counseling (MMSc), and Master of Medical Science Physician Assistant (MMSc-PA).
This group outlined six priority areas of focus that would later serve as the working group structure for the education transformation process (Figure 1):
- Forward-thinking Educational Programming
- Program Evaluation
- Holistic Learner Success
- Educational Experience and Instructional Delivery
- Connectivity and Partnership
- Faculty, Staff, Resident Growth, Development, and Scholarship
One of the initial challenges of this process was recruiting a large number of subject matter experts to volunteer their time to serve on the steering committee. Once formed, this diverse steering committee comprised of thought leaders across health professions education, charged our working groups with developing recommendations for curricular and co-curricular elements to support our vision and goals. Through a series of meetings and retreats with the steering committee, we prioritized and ultimately leveraged recommendations as the basis for the ‘operating principles’ (Figure 2) to guide the next phase of transformation work. See Figure 3 for the process timeline and Figure 4 for an example retreat activity.

DEFINING THE DIRECTION AND DEVELOPING A SHARED UNDERSTANDING
The foundational phase defined the direction of the education transformation process and developed a shared understanding of what the education transformation process aimed to achieve. Objectives of this phase included level-setting across ESOM degree programs by conducting stakeholder mapping exercises and program-specific presentations. Additional objectives were to define the ideal learner development and to understand user needs and challenges by engaging the ESOM community through a series of community Q&A sessions and by conducting surveys of educators and learners. Simultaneously, a review of the relevant literature and compilation of best practices was conducted and disseminated to the working groups. Our biggest challenges at this point were coordinating schedules to facilitate meetings and developing consensus around high level objectives among educators from all six degree programs.
DEVELOPING A PLAN TO SUPPORT IDEAL LEARNERS
Equipped with the stakeholder feedback, national best practices, and an understanding of our current state, the six working groups convened separately to develop recommendations for their unique focus topics. During this phase, the steering committee met monthly to oversee progress and provide feedback on working group findings. The following recommendations set forth by the working groups in March 2023 established the foundation for the ‘operating principles.’
Forward-thinking Educational Programming
- Support learners by providing individualized learning and development based on their needs.
- Teach learners how to work effectively within teams consisting of individuals from other professions, disciplines, and backgrounds.
- Expose learners to new technology areas, artificial intelligence, and teach them how to integrate these technologies ethically and professionally.
Program Evaluation
- Establish program evaluation guiding principles that are transparent and clearly described; to be shared across all programs.
- Communicate ongoing course and curricular updates made in response to evaluations.
Holistic Learner Success
- Center learner wellness as a core consideration by viewing all changes through the lens of improving overall wellbeing of learners.
- Create explicit programming for professional development and wellness.
Educational Experience and Instructional Delivery
- Deliver asynchronous didactic content.
- Emphasize experiential learning through small group/peer-based teaching and problem-solving activities.
Connectivity and Partnership
- Partner and align goals with healthcare partner organizations.
- Develop a set of values to ensure education of learners through interprofessional education.
Faculty, Staff, Resident Growth, Development, and Scholarship
- Create a Department/Center of Education to enable shared resources across all ESOM programs.
- Ensure appropriate training of faculty, staff, and resident educators who teach students in any ESOM program.
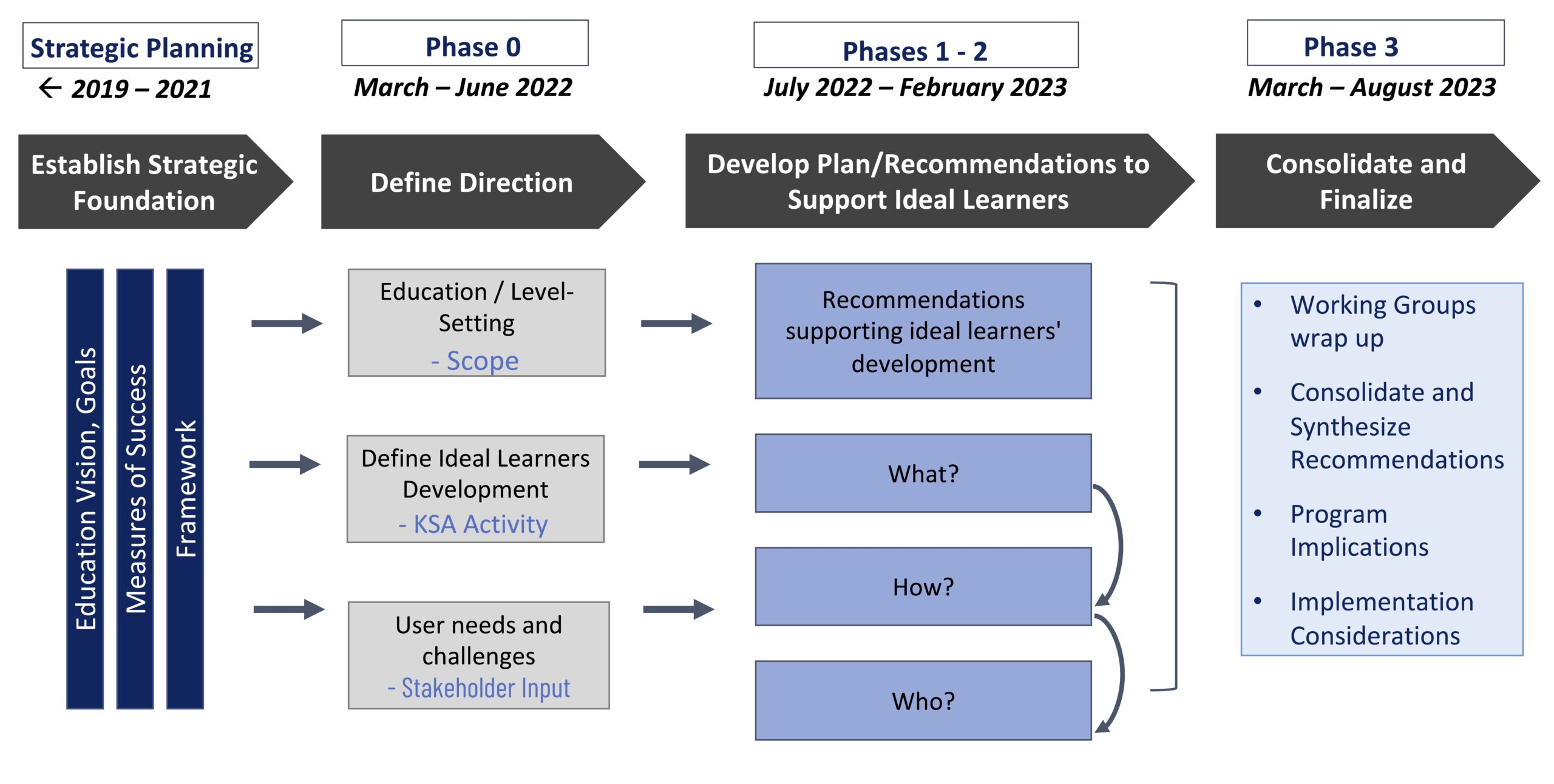

CONSOLIDATING KEY PRINCIPLES
After the working groups made their final recommendations, the steering committee and other key program representatives participated in two retreats with distinct objectives. The first retreat aimed to identify where there are opportunities for shared learning experiences and/or opportunities for shared resources across all ESOM programs. The takeaways from this session resulted in eight common themes prioritized by the participants. The second retreat sought to generate ideas and examples of models of interprofessional experiences within clinical, community, didactic, and simulation settings. During this session, many specific examples of shared learning opportunities were developed across a variety of environments.
Ultimately, we established the key operating principles that will guide our transformation efforts. These include 1) enhancing active learning by curating and developing asynchronous content to support self-directed learning and interdisciplinary teaching and learning, 2) promoting self-directed, life-long learning using activities such as self-assessment of learning needs and identification of effective learning techniques, 3) attending to the ongoing professional development and well-being of our learners, educators, and staff in their roles as teachers through a centralized education resource, and 4) providing interprofessional learning by increasing interprofessional learning activities within didactic, clinical, and community settings. All four of these operating principles are supported by a proposed new shared infrastructure or center for education.
CONTINUED IMPLEMENTATION PLANNING
After the foundational development phases, we recommended the following key activities to build on the momentum of the Steering Committee and other retreat participants:
- Aligning program calendars and curricula mapping – to achieve interprofessional learning experiences to the extent outlined within this report, our programs will first need to align program start dates. To accomplish this, our programs will need to identify where there are similarities and develop curricular structures to advance IPE while also maintaining program-specific requirements and needs.
- Identifying and adopting shared evaluation principles for all programs – developing guiding principles will facilitate evaluation processes that align with each program’s mission and the mission of ESOM.
- Identifying, launching, and assessing outcomes of prototypes and pilots for shared learning experiences – develop and test content and delivery, leveraging examples of IPE experiences developed during this process, as well as other ideas and opportunities that are identified.
- Developing a shared infrastructure plan – articulating and securing the resource needs required to support all programs at ESOM. One concept that was proposed is the creation of a shared ‘Department/Center for Education.’ This concept will continue to evolve as the plan develops.
- Adapting the curricula for the implications of new technologies (i.e. artificial intelligence) in health professions education – developing a shared approach to addressing the presence of artificial intelligence in teaching, patient care, research, and professional development will be critical in the next phase of work.
Towards the end of this lengthy initial process, the ESOM Dean stepped down, creating uncertainty around continuity and ongoing support for the transformation goals. Luckily, prior to stepping down, the outgoing Dean hired a new Senior Consultant for Medical Education Transformation to build the team and infrastructure to operationalize the vision and principles outlined through the transformation process. Continued implementation planning efforts are currently in progress under his leadership with the support of the new Dean and a team comprised of program faculty leaders and other subject matter experts.
CONCLUSION
The recommendations set forth by the working groups and prioritized by the steering committee are intended to be bold and aim to accelerate ESOM’s path from excellence to eminence. Our goal is to graduate excellent clinicians and scientists capable of leading change across complex health systems and communities.
In a bold step, we have involved every program within ESOM in the next iteration of our education transformation, focusing on active learning that meaningfully engages multiple disciplines and community partners. We envision our shared learning model will empower ESOM learners to be change agents capable of addressing evolving health challenges. For additional insights into the process and to review the recommendations report please visit the website
Jada Bussey-Jones, MD
Carter Smith Sr Professor, Department of Medicine, Emory School of Medicine.
Jaimie Keough, MPH
Administrator, Office of Medical Education and Student Affairs.
Pearson Smith, MPH
Manager, Strategic Initiatives, Dean’s Office, Emory University School of Medicine.
Rachel Sedlack-Prittie, MPH
Senior Director, Strategic and Innovation Initiatives, Dean’s Office, Emory School of Medicine
Eric Sundberg, PhD
Professor and Chair, Department of Biochemistry, Emory University School of Medicine