Although proper use of personal protective equipment in medical settings is critical to protecting the health and safety of providers, educational efforts may need to be combined with changes in clinical workflow to improve compliance with published guidelines.
Introduction
In the outpatient oncology setting, contamination of surfaces where hazardous drugs are prepared and administered is common (Hon et al., 2011). Therefore, it is important that healthcare professionals, particularly nurses, use personal protective equipment (PPE) when administering hazardous drugs (HDs) to prevent unintentional absorption via the skin (Smith & Wong, 2018).
As they strive to provide competent and efficient care to their patients, some nurses in the outpatient oncology setting have been observed forgoing PPE use when administering HDs. This decreased use of PPE puts nurses at increased risk for skin rashes, cancer, and reproductive disorders (Connor et al., 2009). It is imperative to preserve and promote the health of frontline healthcare workers by educating and implementing changes that promote increased PPE use. The goal of this practice improvement initiative was to investigate whether an educational intervention would increase proper PPE adherence by nurses while administering HDs in the outpatient oncology setting by 25% over a two-month period.
Methods
This work is a program evaluation that does not constitute human subject research and is therefore exempt from review by the Institutional Review Board.
We chose ten nurses on the outpatient oncology unit at random to observe for this study. The nurses selected had between 3 and 20 years of total nursing experience and 1 to 10 years of experience on the outpatient oncology unit. The selected nurses were observed administering HDs; observations generally took place after 12:00 PM and were conducted between December 1, 2022 and January 30, 2023. Starting February 1, 2023, the same ten nurses were randomly observed again when administering HDs to determine if PPE usage increased or decreased post-education.
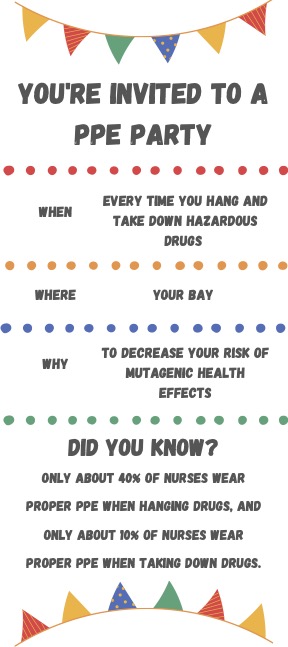
We conducted the first set of observations and did informal interviews prior to developing the educational intervention in order to address the breakdowns in nurses’ proper PPE use and their stated barriers to complying with standards. We then developed the educational intervention which was presented at four separate morning huddles and focused on the importance of donning PPE both when administering and disposing of HDs. The education provided during these huddles consisted of current unit PPE statistics, common ways nurses are exposed to HDs on the unit, and emphasis on the importance of PPE use when administering HDs. We held these sessions once per week for nurses on the unit beginning two weeks into the observation period. We also posted 11 posters promoting proper PPE use throughout the outpatient oncology infusion center at the beginning of the observation period in PPE donning/doffing areas, near time clocks, on the morning huddle board, and at the triage desk (Figure 1).
The study data collection included the pre-educational intervention observations during one work shift of each of the selected nurses as well as one additional observation of each selected nurse approximately 2 months post-intervention. The pre-intervention interviews consisted of two prompting questions: (1) How often do you wear proper PPE when administering/disposing of HDs? and (2) What reasons do you have for not wearing proper PPE when administering/disposing of HDs (if applicable)? A deductive and semantic approach was used to analyze nurse responses to the interview questions.
The observation times for each selected nurse were determined by the treatment regimens of their assigned patients. We evaluated their schedule on their day of observation to determine which of their patients would receive HDs. The nurses were evaluated on proper PPE use when administering and disposing of a selected patient’s HD. For this practice improvement initiative, proper PPE use is considered donning a chemotherapy-resistant gown and 2 pairs of chemotherapy-resistant gloves, as defined by ASTM D6978 specifications (CDC, 2019). A ‘Y’ was given for appropriate PPE use, and an ‘N’ was given for inappropriate PPE use.
Results & Discussion
Results of the pre- and post-intervention observations are shown in Table 1. Before the intervention, 40% (n=4) of the 10 randomly selected nurses were observed wearing proper PPE when administering HDs. Most commonly, when administering HDs, the improperly protected nurses were gowned and wearing only 1 pair of non-chemo-resistant gloves (n=4).
Two months after the intervention was initiated, only 30% of observed nurses wore proper PPE when administering HDs. Of the seven who were improperly protected, six wore a gown and one pair of chemo-resistant gloves and the other wore a gown and one pair of non-chemo-resistant gloves. While the number of study participants who were gowned increased from 9 to 10, and the number who wore any chemo-resistant gloves increased from 6 to 9, the goal of increasing complete compliance with recommended standards by 25% when administering HDs was not met.
Based on the comments we received from the observed nurses prior to our intervention, we assumed that the greatest challenge to improving proper PPE use on the unit would be convincing nurses to change their habits in the face of their everyday workload (Table 2). These comments suggest that issues like time management, burnout, and possibly fixed mindsets could play a role in poor use of proper PPE when administering HDs. Observed nurses reported that having a constant influx of patients with little downtime and limited room in the infusion center led them to forego adherence to proper PPE standards. Throughout the observation period, there was a turnover of 8 nurses whose positions had not been filled by the end of the observation period, which could have exacerbated this issue. Although there was some resistance to change, overall nurses on the unit voiced understanding and respect for the importance of proper PPE use when administering hazardous drugs.
| Participant | Pre-Education: Wearing Proper PPE When Administering HDs | Pre-Education: Wearing Proper PPE When Disposing of HDs |
| 1 | Y | Y |
| 2 | N (gown + 1 pair of non-chemo gloves) | N (only non-chemo gloves) |
| 3 | N (non-chemo gloves only) | N (only non-chemo gloves) |
| 4 | Y | N (only non-chemo gloves) |
| 5 | Y | N (only non-chemo gloves) |
| 6 | N (gown + 1 pair of non-chemo gloves) | N (only non-chemo gloves) |
| 7 | N (gown + 1 pair of chemo gloves) | N (only non-chemo gloves) |
| 8 | Y | N (only non-chemo gloves) |
| 9 | N (gown + 1 pair of non-chemo gloves) | N (only non-chemo gloves) |
| 10 | N (gown + 1 pair of chemo gloves) | N (only non-chemo gloves) |
Table 1: Record of observed nurse PPE use when administering and disposing of hazardous drugs pre-education, and record of observed nurse PPE use when administering HDs post-education.
|
Representative Comments from Observed Nurses About PPE Use |
|
“It’s too hot.” |
|
“I am done having kids.” |
|
“It takes too long to put on/take off.” |
|
“I’m too busy/I have too many patients.” |
|
“I can’t fit into two pairs of chemotherapy-resistant gloves.” |
Table 2. Comments recorded from interviewing nurses on the unit about proper PPE use when administering HDs.
Conclusion
Though the goal of increasing proper PPE use by outpatient oncology nurses when administering HDs was not met with this educational practice improvement initiative, the standard remains critically important for the safety of nurses administering those drugs. The current findings show that while nurses understand the importance of proper PPE use when administering hazardous drugs, there are a variety of barriers that prevent their adherence. The observed nurses proposed decreasing overall patient load and/or increasing available staffing in the outpatient oncology infusion center to allow them time for proper PPE use. We agree, and also propose (1) increasing staffing in the injection clinic connected to the infusion center so that they can provide some of the daily HD injections, and (2) improving workflow to decrease the time between when a doctor/advanced practice provider is paged and when they respond to nurses regarding treatment plan concerns. Delayed call backs from providers impact PPE use by altering nursing workflow. For example, treatment start times for multiple patients can begin to overlap due to delays, which can put pressure on nurses to work quickly.
A positive outcome of this project was that after final observations were completed, a limit was set on the number of patients that can be serviced per day in the outpatient oncology infusion center. Before a limit was set, almost 200 patients could be seen per day. The current limit caps patients at 150 per day. More observations are needed to determine if decreasing the overall patient load has positively affected proper PPE use on the unit. If difficulties with nurse adherence to PPE standards continue, future projects may wish to examine the use of closed system transfer devices (CSTDs) when administering HDs. These devices prevent hazardous drugs from escaping into the environment and decrease surface contamination in the outpatient oncology setting (Smith & Wong, 2018). Proper PPE use in combination with CSTDs will provide the best protection for the safety of outpatient oncology nurses and patients when administering HDs.
Acknowledgments
The author received no grant support for this work and declare they have no conflicts of interest in regard to this work. They also acknowledge: Kallie Palmer, BSN, RN, Abby Cottrell, PA-S1, Laura Pattillo, BSN, RN, MPH, Karly Goozee, MSN, RN, OCN, Courtenay Brown, MSN, APRN, CCNS, PCCN, and Roberta Kaplow, APRN, CCNS, Ph.D., AOCNS, CCRN, FAAN.
Abu Sharour, L., Subih, M., Bani Salameh, A., & Malak, M. (2021). Predictors of chemotherapy safe-handling precautions and knowledge among a sample of Jordanian oncology nurses: A model-building approach. Workplace Health & Safety, 69(3), 115–123. https://doi.org/10.1177/2165079920959991
Centers for Disease Control and Prevention. (2019, May). NIOSH Personal Protective Equipment Information (PPE-Info). Centers for Disease Control and Prevention. https://wwwn.cdc.gov/PPEInfo/Standards/Info/ASTMD697805
Connor, T., Reed, L., Polovich, M., McDiramid, M., Leone, M., & Power, L. (2009). Workplace Solutions – Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/niosh/docs/wp-solutions/2009-106/pdfs/2009-106.pdf
Hazardous drugs – controlling occupational exposure to hazardous drugs. Occupational Safety and Health Administration. (2016). https://www.osha.gov/hazardous-drugs/controlling-occex
Hon, C.-Y., Teschke, K., Chua, P., Venners, S., & Nakashima, L. (2011). Occupational exposure to antineoplastic drugs: identification of job categories potentially exposed throughout the hospital medication system. Safety and Health at Work, 2(3), 273–281. https://doi.org/10.5491/shaw.2011.2.3.273
Lawson, C. C., Johnson, C. Y., Nassan, F. L., Connor, T. H., Boiano, J. M., Rocheleau, C. M., Chavarro, J. E., & Rich-Edwards, J. W. (2019). CE: Original research: Antineoplastic drug administration by pregnant and nonpregnant nurses: An exploration of the use of protective gloves and gowns. The American Journal of Nursing, 119(1), 28–35. https://doi.org/10.1097/01.NAJ.0000552583.69729.51
Roussel, C., Witt, K. L., Shaw, P. B., & Connor, T. H. (2019). Meta-analysis of chromosomal aberrations as a biomarker of exposure in healthcare workers occupationally exposed to antineoplastic drugs. Mutation Research. Reviews in Mutation Research, 781, 207–217. https://doi.org/10.1016/j.mrrev.2017.08.002
Smith, C., & Wong, W. (2018). ASHP guidelines on handling hazardous drugs. ASHP. https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx
Daija Dennis, MN, RN
Nurse Clinician, Winship Cancer Center
Women’s Health & Gender-Related Studies DNP Student, Nell Hodgson Woodruff School of Nursing